To ther Editor,
We present the case of a 79 year-old man diagnosed with high blood pressure and chronic liver disease due to hepatitis C virus. The patient was referred for surgery for severe mitral valve regurgitation associated with the prolapse of P2 and P3 through the spontaneous breakage of the chordae tendineae. The left ventricle (LV) and coronary arteries were normal.
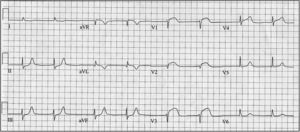
Mitral valve reconstruction was undertaken using a Carpentier-Edwards Physion no. 28 annuloplasty ring and the implantation of two GoreTex cords attached to P2 and P3. No intraoperative complications were encountered. On arrival at the postoperative care unit the patient suffered several episodes of ventricular fibrillation. Advanced cardiopulmonary resuscitation was begun with multiple electrical defibrillations; the situation stabilized following the administration of amiodarone. Emergency bloodwork revealed no ion abnormalities, although an electrocardiogram showed a previously undescribed convex elevation of the ST segment in V1-V3 (Figure 1). Emergency coronary angiography was performed, which revealed the complete occlusion of the conus branch of the right coronary artery (RCA); no such findings were seen in pre-surgery coronary angiography (Figure 2A and B). The left coronary artery tree was normal. After discussing the images with the surgical team it was concluded that the cause of this acute occlusion was a suture used to fix the cable of the epicardial pacemaker in place. Balloon angioplasty was performed and blood flow restored. Good coronary angiographic results were obtained (Figure 2C).
Figure 1. Convex elevation of the ST segment in the right precordial leads.
Figure 2. A: right coronary tree before surgery; non-dominant vessel with no sign of obstruction. B: complete occlusion of the conus branch of the right coronary artery. C: recovery of blood flow in the conus branch following balloon angioplasty.
The first artery arising from the RCA is the conus branch, although in 30%-50% of cases it may originate from the aorta.1 Its function is to irrigate the pulmonary trunk (the outlet tract of the right ventricle [RV]). When very developed it can reach as far as the lateral wall of the RV. Its acute occlusion, either because of vasospasm (the most common cause), atherosclerotic disease or accidental injury during surgery in the region of the pulmonary infundibulum, etc., can give rise to myocardial ischemia in the latter area and in the RV lateral wall. This is manifested by two major events. The first is ST segment elevation in the right precordial leads, which has also been described in isolated ischemia of the RV. Geft et al.2 concluded that, after inducing ischemia in experimental animals, the isolated involvement of the RV (i.e., with no LV involvement) gives rise to the displacement of the electrical forces towards the right, and thus ST segment elevation for these leads. However, when the LV is involved (generally the inferoposterior segments), left forces predominate and ST segment elevation is seen in the leg leads accompanied by ST segment depression in the right precordial leads. The second is a greater predisposition towards suffering polymorphic ventricular tachycardia and/or ventricular fibrillation. In animal models it has been shown that ischemia of the RV outlet tract leads to abnormal action potentials in the epicardial cells. This induces a greater dispersal of the repolarization wave, which precipitates ventricular arrhythmias through re-entry mechanisms during phase 2 of the action potential.3 This mechanism is similar to that seen in patients with Brugada syndrome, and cases have been reported in which ischemia in this territory, generally due to vasospasm, has caused ventricular arrhythmias.3, 4.
In conclusion, the occlusion of the conus branch of the RCA by vasospasm or other mechanisms can cause myocardial ischemia in the region of the pulmonary infundibulum and the lateral wall of the RV, and ST segment elevation in the right precordial leads. The risk of arrhythmia generated by a mechanism similar to that seen in Brugada syndrome is high. It is essential that the surgeon know the origin and trajectory of the conus branch of the RCA before operating.
.
Corresponding author: [email protected]